Why We Need a ‘Digital Health Data Safety Net’
Lessons from Meaningful Use on achieving digital equity for all providers
This year has felt like the start of another seismic shift in healthcare infrastructure. The Trusted Exchange Framework and Common Agreement (TEFCA) is advancing nationwide exchange and interoperability by designating an initial set of Qualified Health Information Networks (QHINs) to connect existing and emerging networks and expand health data exchange.
The Center for Medicare & Medicaid Services is set to finalize requirements for health plans to further streamline and modernize prior authorization and data sharing with providers and other plans through FHIR APIs. Many states are emerging from the pandemic with initiatives to transform both public health and Medicaid — initiatives that depend on data sharing across the healthcare ecosystem and with public health — to achieve health equity, preparedness, and whole person care goals. In our state, California is actively implementing its first statewide health data exchange framework, requiring most healthcare entities to exchange health information by 2024. With this wave of policy changes, and some actual enforcement teeth for the 21st Century Cures Act Information Blocking Rule that prohibits intentional interference with health data sharing, things might be changing…fast.
The last time we had a seismic shift in health IT of this scale started in 2009 with the ARRA economic stimulus plan setting out $27 billion in incentives to help medical organizations adopt electronic health record (EHR) technology. Included in the details of the Health Information Technology for Economic and Clinical Health (HITECH) Act were specifics around determining “Meaningful Use” of the technology to grant financial incentives. Meaningful Use (MU) was designed to create a digital health revolution, to move us off paper records and on to computers. By many measures, the program was highly effective, introducing an extraordinary amount of change in a very short period of time. In the course of 10 years, EHR adoption in hospitals went from 9 percent to 96 percent thanks to the program, and from 48 percent to 88 percent among office-based physicians.
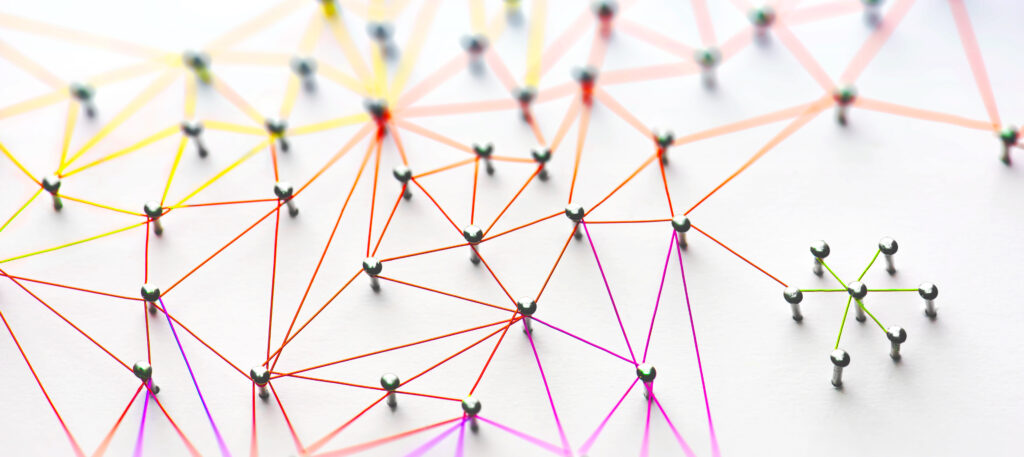
However, interoperability and seamless data sharing between those digital systems was deprioritized in favor of driving basic EHR adoption and use: We built the houses and businesses through the MU program, but we failed to plan and invest adequately in the roads that connect them. And while the MU program incorporated a few health information sharing and public health measures, the financial investment in interoperability infrastructure through the one-time State HIE Cooperative Agreement Program (HIE Program) of $564 million — 2 percent of the amount invested in the MU program divvied up across 50 states and a handful of territories — simply wasn’t enough to enable the robust, durable “roads” we need.
Read the full article published in Healthcare Innovation.